Reminder – Prior Authorization/Treatment Authorization Fields
| Date: | December 9, 2022 |
| To: | HPSJ Contracted Providers and Facilities |
| From: | Health Plan of San Joaquin (HPSJ) |
| Type: | Regulatory/Informational |
| Subject: | Reminder – Prior Authorization/Treatment Authorization Fields |
| Business: | Medi-Cal Managed Care |
The Health Plan of San Joaquin (HPSJ) Claims Provider Disputes Resolution team has identified an increase of requests related to Appeals of Medical Necessity/Utilization Management Decision for Outpatient and Professional Services. It has been identified that prior authorization has been obtained however not billed in the required fields. If an authorization is required, it must be billed on the claim for proper reimbursement. If no authorization is required, the field must be left blank to avoid, invalid authorization denials.
If a denial is received, a resubmission of the claim with the correct/additional information is required using the Corrected Claim Process. Do not submit a Provider Dispute Resolution (PDR).
Please go to www.hpsj.com/wp-content/uploads/2021/05/HPSJ-provider-billing-guide.pdf for additional information on how to submit a corrected claim.
Below are examples of where to submit the authorization number for either paper form or electronic 837 format.
UB04 Example:
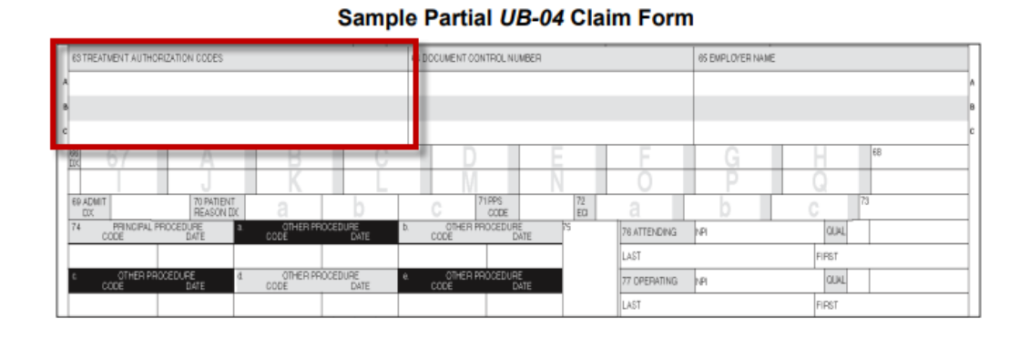
Please see page two for additional examples regarding the 837 formats.
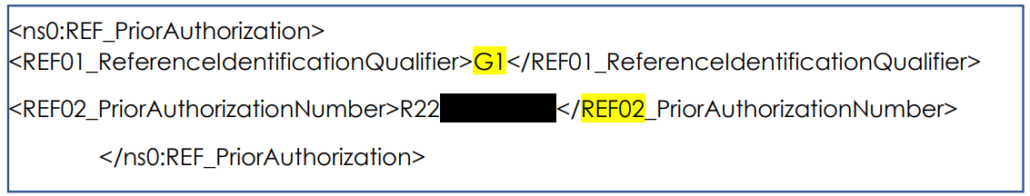
837 I Example: Loop 2300 Ref/GI/02
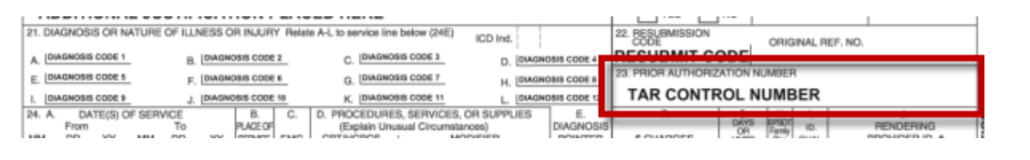
CMS1500
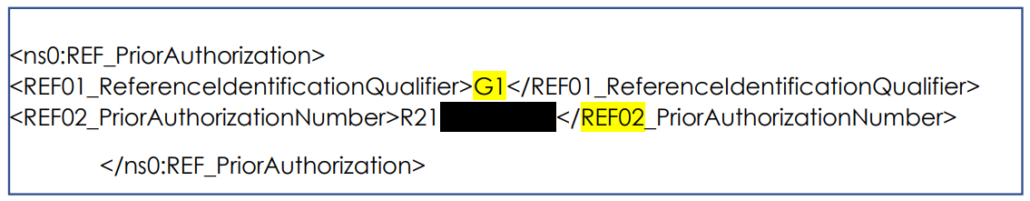
837P Example: Loop 2300 Ref/GI/02
If you have any further questions, please contact your Provider Services Representative, or call our Customer Service Department at 1-888-936-PLAN (7526). You may also visit www.hpsj.com/alerts for online access to the documents shared.

