Medi-Cal Pharmacy (Rx) Update – Phase IV, Waves 1, 2, 3, Enteral Nutrition
| Date: | October 17, 2023 |
| To: | Health Plan of San Joaquin (HPSJ) Practitioners and Facilities |
| From: | HPSJ |
| Type: | Informational/Educational |
| Subject: | Medi-Cal Pharmacy (Rx) Update – Phase IV, Waves 1, 2, 3, Enteral Nutrition |
| Business: | Medi-Cal Managed Care |
Outpatient pharmacy benefits were transitioned to Medi-Cal Rx on 1-1-2022. Due to the
benefit transitioning, some medications are paid for by Medi-Cal Rx and some are paid for by the Health Plan of San Joaquin (HPSJ). Medi-Cal Rx and HPSJ may request providers to bill specific injectable medications to Medi-Cal Rx. The Medi-Cal Rx Provider Manual also (https://medi-calrx.dhcs.ca.gov/cms/medicalrx/staticassets/documents/provider/forms-and-information/manuals/MediCal_Rx_Provider_Manual.pdf) provides further details of medications and DME covered by Medi-Cal Rx.
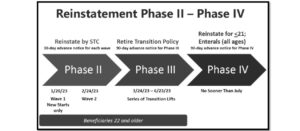
EFFECTIVE August 4, 2023, the first wave of Phase IV went live in which “Reject Code 60 – Product/Service Not Covered for Patient Age,” “Reject Code 61 – Product/Service Not Covered for Patient Gender,” and “Reject Code 606 – Brand Drug/Specific Labeler Code Required” claim edits were reinstated. Specific details can be found at the following page: https://medi-calrx.dhcs.ca.gov/cms/medicalrx/static-assets/documents/provider/bulletins/2023.07_A_30-Day_Countdown_Phase_IV_Lift_1.pdf
EFFECTIVE September 22, 2023, the second wave of Phase IV goes live in which “Reject Code 78 – Cost Exceeds Maximum” claim edits will be reinstated. Three therapeutic classes (protein lysates, infant formulas, and electrolytes and miscellaneous nutrients), including new start of enteral nutrition products will also require Prior Authorization for patients 22 years of age and older. Specific details can be found at the following page: https://medi-calrx.dhcs.ca.gov/cms/medicalrx/static-assets/documents/provider/bulletins/2023.08_A_30-Day_Countdown_Phase_IV_Lift_2.pdf
EFFECTIVE October 13, 2023, the third wave of Phase IV goes live in which “Reject Code 76 – Plan Limitations Exceeded” claim edits will be applied to all new start claims for all ages and all refill claims for members 22 years of age and older. Specific details can be found at the following page: https://medi-calrx.dhcs.ca.gov/cms/medicalrx/static-assets/documents/provider/pharmacy-news/2023.09_A_30-Day_Countdown_Phase_IV_Lift_3.pdf
EFFECTIVE November 9, 2023, the Transition Policy will be retired and all enteral nutrition orders for members 22 years of age and older will require Prior Authorization. Specific details can be found at the following page: https://medi-calrx.dhcs.ca.gov/cms/medicalrx/static-assets/documents/provider/bulletins/2023.08_A_90-Day_Countdown_Reinstatement_PA_Requirements_Enteral_Nutrition_Claims_Members22Years_Older.pdf
Medi-Cal Rx has also created a dedicated reinstatement web page that will provide weekly updates regarding Phases II, III, and IV. The web page can be found at https://medi-calrx.dhcs.ca.gov/home/education/ and then selecting the “Medi-Cal Rx Reinstatement” tab. The specific list of therapeutic classes that will be reimplemented with each phase/wave can also be found in this tab in the resources section.
In the event that a dispensing pharmacy obtains a “Reject Code 816 – Pharmacy Drug Benefit Exclusion” notification when billing to Medi-Cal Rx, the pharmacy or provider may submit a PA request to Medi-Cal Rx for consideration of an exception to bill the drug through the pharmacy benefit. If Medi-Cal Rx continues to deny coverage through the pharmacy benefit, consideration by the provider should be made to submit a PA to HPSJ for consideration of coverage under the medical benefit.
Methods to distinguish whether a medication would be billed through the Pharmacy Benefit (billed to Medi-Cal Rx), or the Medical Benefit (billed to HPSJ) are listed below.
Pharmacy Benefit – Medication is processed through a Pharmacy Benefit Manager (PBM) at a dispensing pharmacy location. This applies to the following sample pharmacy types: retail, specialty, long-term-care, mail-order, compounding, etc. If a PA is required then visit https://medi-calrx.dhcs.ca.gov/cms/medicalrx/staticassets/documents/provider/bulletins/2022.01_A_PA_Submission_Reminders.pdf for various methods to send a PA to Medi-Cal Rx.
Medical Benefit – Medication is already currently in stock at the provider’s office (buyand bill) or within the facility administering the medication (e.g. outpatient infusion centers). If a PA is required then send a Medical Authorization form to HPSJ – https://www.hpsj.com/wp-content/uploads/2022/09/Medical-Authorization-9_2022-updated_fillable.pdf.
Pharmacy Benefit (Medi-Cal Rx) |
Medical Benefit (HPSJ) |
|
|---|---|---|
| All Retail Pharmacies (e.g. CVS, Walgreens, independent pharmacy) | Yes | No |
| Specialty Pharmacy (e.g. Accredo, Diplomat, Optum, US Bioservices) mailing to the patient or to the provider’s office on behalf of the patient | Yes | No |
| Long-term-care pharmacy is filling the medication and sending it to the Skilled Nursing Facility | Yes | No |
| Provider or Facility already purchased and has the medication in their office/facility with plans for infusion or injection at their office/facility | No | Yes |
| Outpatient infusion center using medications from within their internal stock and planning for infusions at their site | No | Yes |
 For any further questions that Medi-Cal Rx is unable to assist in resolving, please contact the HPSJ Pharmacy Department at 209.461.2212 to leave a secure voicemail that will be returned within one business day.
For any further questions that Medi-Cal Rx is unable to assist in resolving, please contact the HPSJ Pharmacy Department at 209.461.2212 to leave a secure voicemail that will be returned within one business day.

