2022 Quality Measures for FQHC & RHC- UPDATED (This Supersedes alert sent on 12/29/2021)
| Date: | February 17, 2022 |
| To: | All HPSJ Federal Qualified Health Center (FQHC); Rural Health Clinics (RHC) |
| Provider Alert Type: | Informational/Educational and Procedural Update |
| From: | Health Plan of San Joaquin |
| Subject: | 2022 Quality Measures for FQHC & RHC- UPDATED (This Supersedes alert sent on 12/29/2021) |
| Business: | Medi-Cal |
Health Plan of San Joaquin (HPSJ) is pleased to announce the 2022 Provider Incentive Program promoting Quality Care to our members. The requirements for participation include the following qualifiers:
2022 Qualifiers to Participate
1. Maintain a minimum of 500 HPSJ members per assigned provider
2. Clinic(s) must remain open to new members the entire calendar year
The Quality Measures include Healthcare Effectiveness Data and Information Set (HEDIS) and the Managed Care Accountability Sets (MCAS) – performance measures that the Department of Health Care Services (DHCS) selects for annual reporting by Medi-Cal managed care health plans. Please note that DHCS has put an extra emphasis on children’s well care measures for 2022.
2022 Quality Measures for FQHC/RHC
• BCS – Breast Cancer Screening
• CCS – Cervical Cancer Screening
• CIS – Childhood Immunization Status Combination 10
• CBP – Controlling High Blood Pressure
• HBD-A1c Poor Control – Diabetic patients with A1c >9 (lower is better)
• CHL -Chlamydia Screening in Women
• IMA – Immunizations for Adolescents Combination 2
• LSC – Lead Screening in Children
• PPC Pre – First Routine Prenatal Care Visit (within timeframe)
• PPC Post – Post Partum Visit (1-84 days after delivery)
• IHA – Initial Health Assessment – within 120 days of new member enrollment
• W30- Well Child Visit in first 30 months; 6+ Visits by 15 months; 2+visits 15-30 months
• WCV – Child and Adolescent Well Child Visits
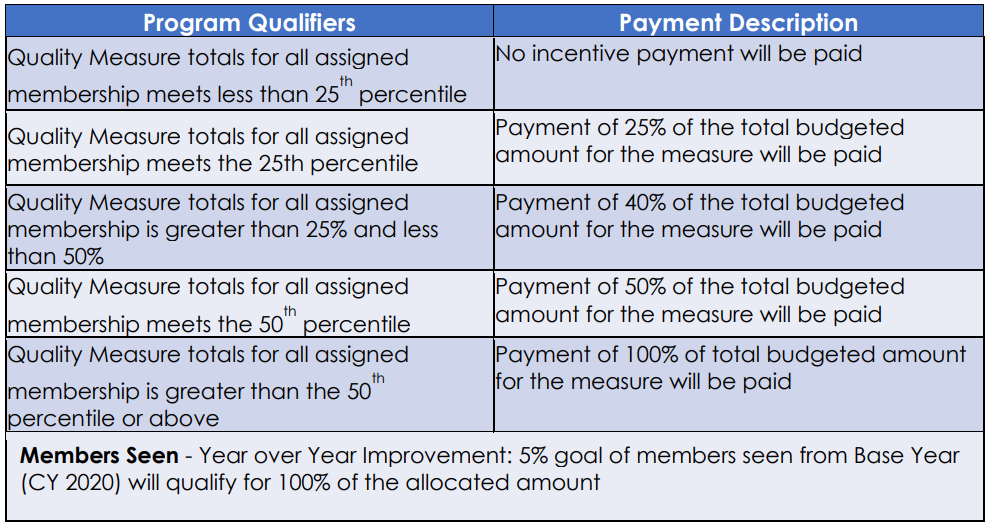
- Funding pool for each participating clinic is allocated based proportionally to the membership served and distributed equally for each measure achieved.
- 10% of the funding pool is reserved for clinics that can demonstrate year over year improvement with the percentage of members seen from the previous year.
Each participating clinic organization has a customized “Membership Seen” goal. 90% of the funding pool is to be paid for successful measures met.
HPSJ looks forward to our continued partnership in providing high quality care to our members. Your engagement as a provider not only helps HPSJ members receive care, but it also helps us improve the health status of the overall community.
We appreciate your work and continued partnership. If you have questions, please contact your Provider Services Representative, directly or Customer Services at 888.936.7526.

