Update – DHCS APL 20-010 Cost-Avoidance, Other Health Coverage, and Post Payment Recovery
| Date: | December 11, 2020 |
| To: | Health Plan of San Joaquin (HPSJ) All Providers & Facilities |
| From: | Health Plan of San Joaquin |
| Subject: | Update – DHCS APL 20-010 Cost-Avoidance, Other Health Coverage, and PostPayment Recovery |
| Business: | Medi-Cal Managed Care |
State law requires Medi-Cal and Managed Care Plans (MCPs), such as HPSJ, to be the payer of last resort for services in which there is a responsible third party.
What does this mean for HPSJ providers?
HPSJ members with Other Health Coverage (OHC) must utilize their OHC for covered services prior to accessing their Medi-Cal benefits.
In accordance with All Plan Letter (APL) 20-010, beginning January 1, 2021 HPSJ and its delegates must include OHC information in a notification to the Provider when a claim is denied due to the presence of OHC.
Beginning January 1, HPSJ will begin with the following processes:
- •When a claim is denied due to OHC, requiring Providers to first bill the primary health coverage and then HPSJ as the secondary payer:
- Providers will be directed to our secured portal via the remittance advice or 835 files. HPSJ should be billed as the secondary carrier once the primary payer has made a payment or denial determination.
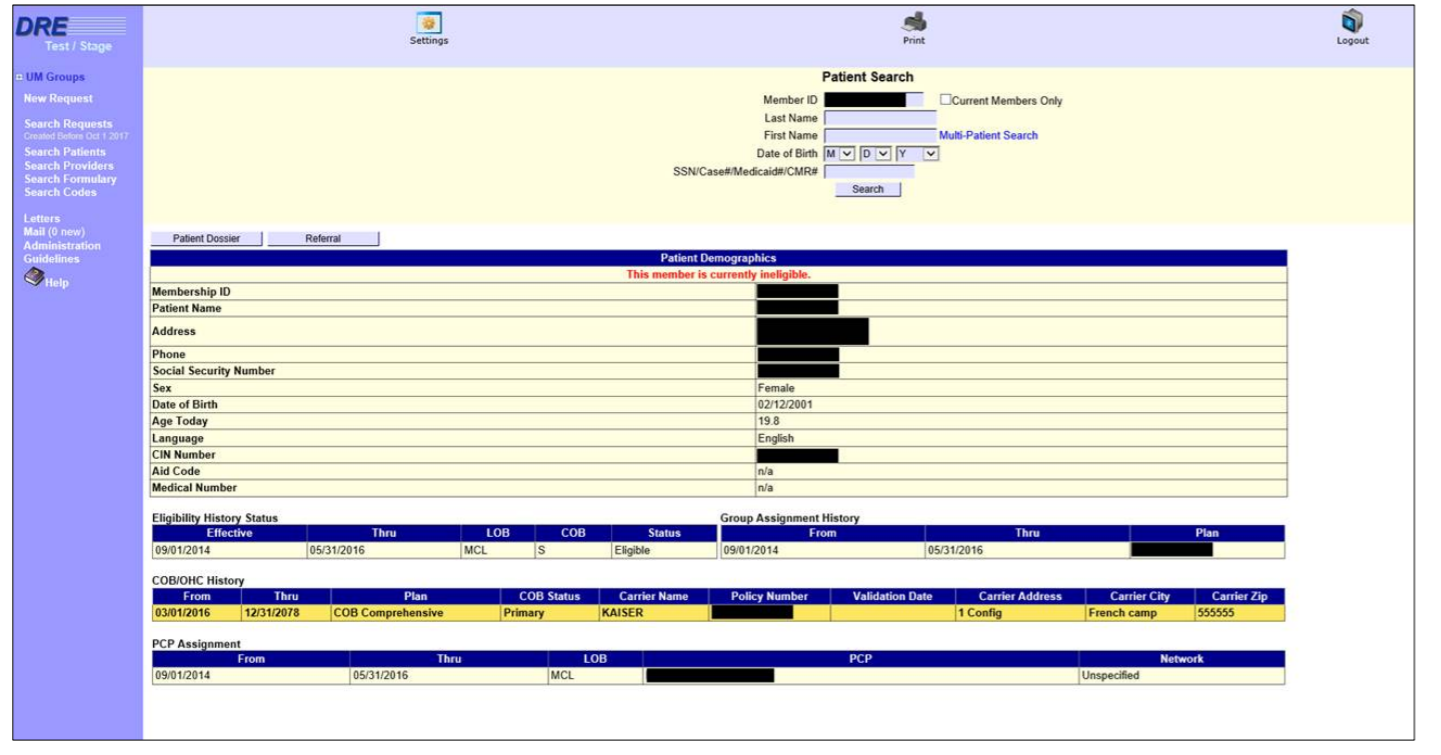
- Robust eligibility verification record of Other Health Coverage (OHC) will be available via our enhanced Doctor’s Referral Express (DRE) provider portal.
If you have questions, please contact our Customer Service Department at 209-942-6320.

